Current statistics by the National Institute of Mental Health (NIMH) suggest that nearly 1 in 5 U.S. adults live with some form of mental illness (NIMH, 2019). This means that nearly 46.6 million Americans over the age of 18 struggle with some form of diagnosable mental illness ranging in severity from mild to severe. Prevalence rates of mental illness are not distributed equally, however, as the data suggests that females suffer more from mental illness than males (22.3% and 15.1% respectively) and that Caucasians report the highest rates of mental illness (20.4%) relative to other races and ethnicities. Younger adults ages 18–25 appear to have the highest incidence rates of mental illness (25.8%) among the adult population. Unfortunately, fewer than half of those suffering with mental illness will receive any form of treatment. Treatment numbers also appear highly impacted by ethnicity and socioeconomic status, with Caucasians receiving treatment at the highest rate (48%) and Asian Americans receiving the lowest (20.2%). Mental illness rates for adolescents is also alarming with approximately 22% of adolescents ages 13–18 suffering from some form of diagnosable mental illness (NIMH, 2019). Additionally, 50% of all lifetime cases of mental illness develop by age 14 and 75% by age 25, suggesting that early intervention is crucial to mitigate later dysfunction and loss of productivity.
The rate of suicide in America is a particular tragedy. Currently, suicide is the second leading cause of death among 10- to 34-year-olds, the fourth leading cause of death among 35- to 54-year-olds, and the 10th leading cause of death overall (NIMH, 2018). Moreover, suicide rates have increased by 28% between 1999 and 2016, claiming the lives of nearly 47,000 people in 2017 alone. The increasing rate of suicide and deaths resulting from accidental overdose and chronic alcoholism — now referred to as “deaths of despair” — have decreased the mean life expectancy in America for the first time since World War I and the ensuing Spanish Flu pandemic.
It’s difficult to talk about the rates of mental illness and suicide without mentioning the impact of substance abuse and alcoholism. The NIMH reported in 2014 that over 20 million Americans have a diagnosable substance use disorder with nearly 8 million having both a substance use disorder and another type of mental illness. We refer to the combination of two or more disorders as “co-morbidity,” which significantly exacerbates the complexity of treatment. Additionally, substance abuse is a frequent component of suicide; between 40% and 75% of those who commit suicide are either under the influence at the time of death or using substances to intentionally end their lives.
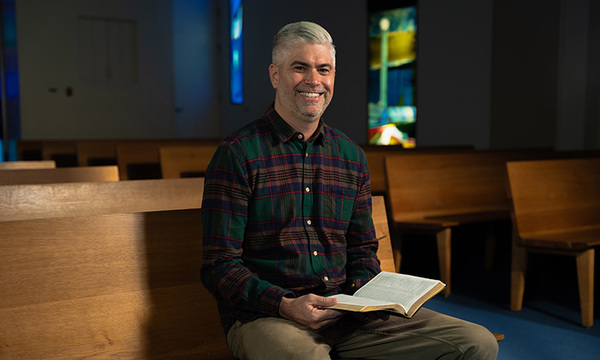
So, how do these alarming statistics impact the modern church and the role of its leaders? The good news is that there is considerable evidence to suggest that church attenders experience significantly higher levels of mental health and emotional well-being (Harvard Institute for Natural Healing, 2016). Additionally, Protestants and Catholics (as well as those of other religious faiths) have historically demonstrated a lower rate of suicide than the secular community. However, the hard truth is that the current mental health crisis and suicide epidemic has certainly not bypassed the church entirely. The remainder of this article will describe the nature of the current mental health crisis in America and some questions for the pastor or ministry leader to consider to maximize the church’s impact on the well-being of those who participate in their ministry.
WHAT’S CAUSING THE RAPID INCREASE IN MENTAL ILLNESS?
The sudden increase in rates of mental illness in America have generally caught mental health professionals and policy makers off guard. Indeed, there is little consensus among the psychological community as to the reason(s) behind the increase, and there are no adequate resources in place to respond. Perhaps the most agreed upon proposition is that it’s quite unlikely that only one issue or societal shift is having such a broad impact on the population. My clinical work with Christian and non-Christian patients tends to suggest the same conclusion: multiple and varied factors appear to be influencing declining mental health rates. Suggested causes that are consistent with my anecdotal clinical experiences include: the growing impact of social media and the “always on” culture; lack of substantive community; secularism and a growing sense of existential despair and hopelessness; 24/7 news and the resulting vicarious trauma; delayed maturation, particularly for males; unreasonable academic and performance expectations; poor diet; and aggressive political division.
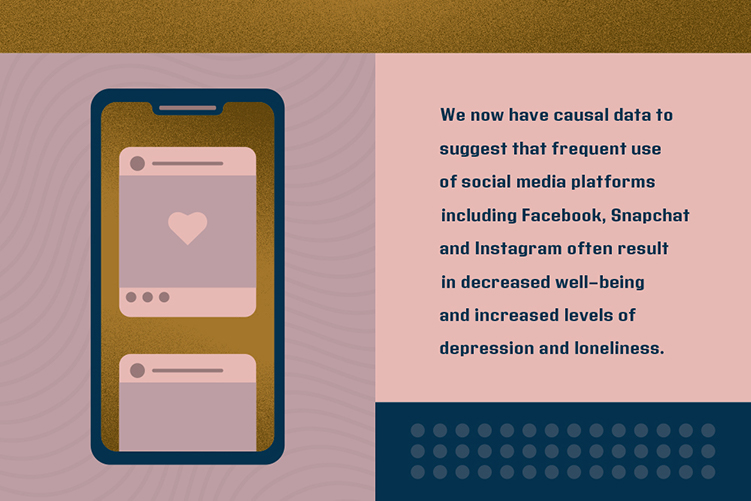
We now have causal data to suggest that frequent use of social media platforms including Facebook, Snapchat and Instagram often result in decreased well-being and increased levels of depression and loneliness (Journal of Social and Clinical Psychology, 2018). Modern neuroimaging reveals that three primary networks are activated while using social media: the “mentalizing network,” the “self-referential network” and the “reward network,” and it may be instructive as to why the frequent use of social media decreases well-being. Neuroimaging results indicate that social media use doubles the amount of time we spend thinking about ourselves (self-referential network) when compared to typical speech and that the reward network of the brain doles out increasing amounts of dopamine when our posts are “liked” or responded to (Healthy Penn State, 2018). Researchers suggest that continuous social comparison and fear-of-missing-out (FOMO) is particularly difficult for adolescents and young adults to manage and suggest that a quick way to improve well-being is to “put your phone down and be with the people in your life.” Along with the many benefits of social media come serious emotional hazards when used in a mindless or indiscriminate manner.
Another area of struggle I commonly see in my patients is what’s referred to as “technostress,” which refers to the negative impact technology usage has on individuals. We live in an “always on,” hyperconnected culture in which work can be done 24/7, and there are virtually no limits on when one can be contacted. Email, text messages, social media notifications, chat, etc., are an ongoing source of fun, demand, work and stress.
Very few of us manage these mediums with self-discipline and often describe significant and continuous distraction and techno-fatigue. Recent research suggests that just the proximity of our smartphones creates distraction. A smartphone that is face down on the table during a meeting creates much more distraction than a phone that is either in our pocket or outside of the room. The smartphone not only induces distraction merely by its presence, it also reduces cognitive capacity resulting in a type of “brain drain” that limits one’s availability to engage in the cognitive task at hand. Researchers report a decreased sense of happiness, accomplishment and connectedness when our autonomic attentional systems are disrupted by the non-conscious cognitive demands of a nearby smartphone (Journal of the Association for Consumer Research, 2017). Again, smartphone technology has been a source of great convenience and connection, however, misuse and an inability to contain its usage may result in decreased levels of well-being and elevated stress and anxiety.
A lack of substantive community is a source of great pain for many in modern American culture. Multinational governmental agencies in the U.S., U.K. and beyond are describing it as a “loneliness epidemic” (Harvard SITN, 2018). A survey of 20,000 U.S. adults conducted in 2018 by Cigna Healthcare found that nearly half of Americans sometimes or always feel alone or left out. Only 53% of respondents report that they experience meaningful social interactions on a regular basis. Generation Z (adults ages 18–22) reports that they are the loneliest generation and appear to be in worse physical health than older generations. The research associating loneliness with decreased physical health is well established. As a result, former U.S. Surgeon General Dr. Vivek Murthy suggests that elevated feelings of loneliness may create health vulnerabilities comparable to smoking 15 cigarettes per day (2018). Church communities including care ministries, small groups and community groups can be a profound antidote to the loneliness phenomenon. The church is uniquely placed to respond with the love of Christ and fellowship to the lonely and quietly displaced.
A particularly unique role the church is called to fulfill is that of a counter-voice to our culture of secularism that is laced with a growing sense of existential hopelessness and despair. As I write this, the news is filled with stories from three mass shootings in seven days resulting in over 100 casualties. This is grim news indeed, but also highlights the role of “vicarious trauma” in the lives of normally unimpacted individuals. One unintentional result of 24/7 news feeds is that our brains are frequently inundated with images and stories of trauma. Tragic events from near and far are experienced in nearly real-time and tend to invade innocuous social media stories and home pages. Unfortunately, the human brain is not very adept at differentiating another’s traumatic experiences from one’s own, resulting in a heightened state of arousal and stress that is physically and emotionally destructive over time. God did not design our bodies and minds to be in a state of nearly continuous hyperarousal, and current technologies may unnecessarily activate the brain’s natural threat detection mechanisms, leading to exhaustion, cynicism and despair. Humans need to manage the inflow of information — particularly threatening or terrifying news — that is not actionable or proximate to maintain a groundedness in one’s actual reality.
Emotional well-being and mental health are correlated to one’s physical health. Few people are at their best psychologically when experiencing ill-health or chronic pain and discomfort. The field of health psychology takes a multidisciplinary approach to well-being that addresses the state of one’s body, mind and spirit (Mark 12:30). This more recent research indicates what we tend to know intuitively: the state of one’s mind, body and spirit interact and impact each other. As a result, mental health is intricately linked to physical and spiritual health. This seems particularly important in modern America as we are confronting an obesity epidemic combined with an increasingly sedentary lifestyle.
The church is obviously positioned to attend to people’s spiritual well-being, but is it possible for the church to meaningfully respond to the flock’s physical health?
Here’s an idea: I recently heard of an associate pastor who purchased used exercise equipment and created a workout gym in an underutilized room on the church campus. He invited cohorts of congregants categorized around age and condition to work out multiple times per week. This ministry has grown exponentially and has been particularly appealing to the older adult population within the church. Exercises for older adults are as basic as sitting down on the floor and then getting back up. These exercises have helped older adults transition from nearly sedentary (and isolated) lives to walking more effectively and, perhaps equally important, interacting multiple times per week with others in their community. In fact, the older adults have had such a positive experience that they have funded the purchase of more equipment. This is a wonderful example of how the church can capitalize on what we know about the interconnectedness of the mind, body and spirit.

HOW CAN THE CHURCH RESPOND?
Although the majority of this article has focused on the realities of America’s current mental health crisis, I want to conclude with a few thoughts on how the church can proactively and effectively respond. First and foremost, the church is uniquely positioned to take a leading role in caring for those who struggle emotionally and psychologically. Lifeway Research suggests that 67% of Christians describe their church as supportive relative to their mental health issues. Additionally, a significant majority of those who attend church even occasionally will seek out counsel from their pastor prior to seeking care from a mental health professional. This is encouraging data and suggests that the church and pastors are increasingly being seen as a safe environment for congregants to bring their mental health struggles.
For the Christian community, pastors and lay leaders are on the frontlines of triaging, counseling and resourcing congregants with mental health concerns. Effectively responding to this aspect of your call will require ongoing training that is congruent with your position in ministry. Such training may include continuing-education-type courses, whether online or in person, consultation with trusted Christian mental health professionals in your community, reviewing current research and books that specifically address issues related to mental health and the church, and an exploration of what other churches are doing to address their congregants’ mental health needs.
Likewise, researching and implementing potential care ministries that are directly, or indirectly, oriented toward those who may be struggling emotionally can also be an effective way to proactively and reactively respond to those within and outside of your church communities and to assist in reducing the stigma attached to such needs. Well-known care ministries such as Celebrate Recovery, GriefShare, DivorceCare, DivorceCare for Kids, short-term or lay counseling programs such as Stephen Ministries, Mothers of Preschoolers (MOPS), exercise ministries as mentioned earlier and specific mental health-oriented support groups and care ministries can have a profound effect upon the well-being of your congregants. Churches such as Saddleback Church in Orange County, Calif., have developed a variety of specific mental health care ministries and sell pre-packaged, supporting materials and online instructions for a nominal fee.
Lastly, if you are a pastor, it is imperative to remember you are equally vulnerable to each of the struggles mentioned in this article. You already know that pastoring is a complex, demanding and little understood profession with a high potential for burnout and mental and physical exhaustion. In fact, the data suggests that, as pastors, you are at a slightly higher risk for mental health issues than the broader population. Caring for your own health and emotional well-being is perhaps best thought of as stewardship of your body and mind (1 Cor. 6:19–20) — and your well-being is a fundamental ingredient in being able to care for the well-being of others and a necessary pursuit to thrive in ministry long term.
For more readings on this topic:
Counseling and Mental Health in the Church: The Role of Pastors and the Ministry, by Kevin Van Lant and Robyn Bettenhausen Geis (Cognella Academic Publishing, March 2019)
Finding Quiet: My Story of Overcoming Anxiety and the Practices that Brought Peace, by J. P. Moreland (Zondervan, May 2019)
Grace for the Afflicted: A Clinical and Biblical Perspective on Mental Illness, by Matthew S. Stanford (IVP Books, September 2017)
American Psychosis: How the Federal Government Destroyed the Mental IllnessTreatment System, by E. Fuller Torrey (Oxford University Press, October 2013)
 Biola University
Biola University